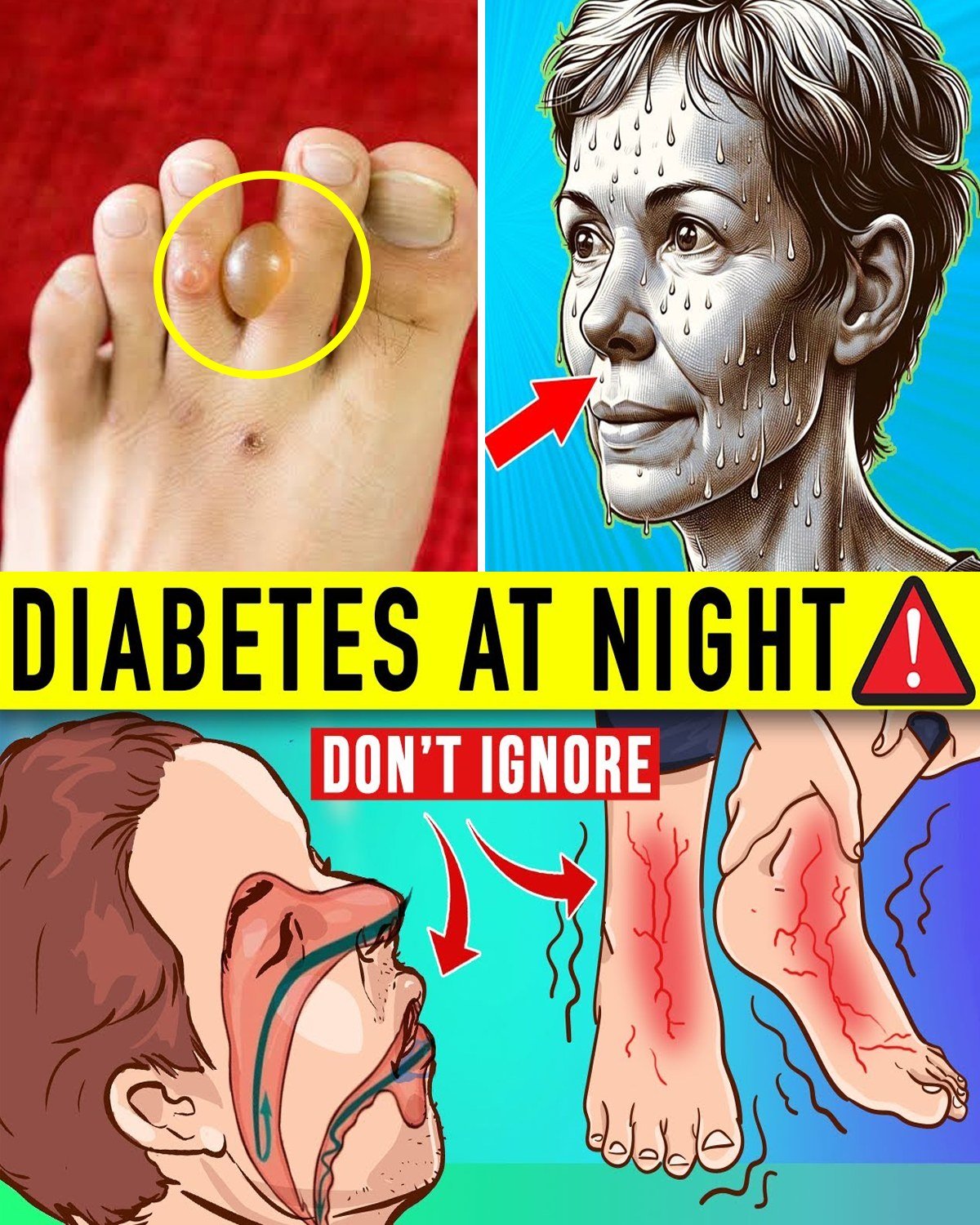
7 Dangerous Nighttime Signs of Diabetes You Need to Know Before It’s Too Late
Did you know that over 37 million Americans have diabetes, and nearly 1 in 4 don’t even know it yet? Many discover it through subtle nighttime symptoms that disrupt sleep and signal serious blood sugar imbalances.
Imagine this: You drift off feeling okay, but hours later you’re soaked in sweat, legs twitching uncontrollably, or rushing to the bathroom for the third time. It’s exhausting—and potentially dangerous. Rate your sleep quality on a scale of 1–10 right now (1 being restless and interrupted, 10 being deep and refreshing). Hold that number.
If you’re over 45, have a family history of diabetes, or carry extra weight, you’ve probably wondered if those midnight wake-ups are “just aging.” What if they’re early warnings your body needs better blood sugar control? Stick around as we uncover 7 critical nighttime signs that could indicate uncontrolled diabetes—backed by science, real stories, and practical steps to reclaim restful nights.
Why Nighttime Symptoms Matter So Much in Diabetes
Diabetes doesn’t clock out when the sun sets. In fact, nighttime is when blood sugar fluctuations can become most dangerous—because you’re asleep and can’t respond quickly. Research shows poor sleep in diabetes worsens insulin resistance, raises A1C levels, and increases complication risks.
It’s frustrating: You eat right, take meds, yet wake up drained. Sound familiar? These signs often stack: one leads to another, creating a cycle of fatigue, mood dips, and even higher heart risks.
Have you paused to count how many times you wake at night? If more than once, this could be a red flag.
You’ve probably tried melatonin, cutting caffeine, or white noise—yet the issues persist. Why? Because treating symptoms without addressing blood sugar misses the root.
But what if recognizing these patterns could transform your sleep—and health? The journey starts now.
Night Sweats: The Silent Blood Sugar Alarm
Let’s begin with a common yet overlooked sign.
Why it happens: Nocturnal hypoglycemia (low blood sugar) triggers adrenaline surges, causing profuse sweating even in a cool room.
Real story: Susan, 58, a school administrator from Texas, woke drenched nightly. Her doctor adjusted her evening insulin. Within two weeks, sweats stopped. “I finally sleep through the night,” she shared.
Science note: Studies link nighttime lows to increased heart strain.
What to do: Check blood sugar before bed. Keep fast-acting carbs bedside.
Rate your night sweats frequency 1–10. If above 3, pay attention.
Restless Legs Syndrome: The Neuropathy Connection
Number six: legs that won’t stay still.
Mechanism: High blood sugar damages nerves (peripheral neuropathy), causing tingling and urges to move.
Safe strategy: Maintain steady glucose. Gentle evening stretches or warm baths help.
Pro tip: Cut caffeine after noon.
Nocturnal Hypoglycemia: The Hidden Midnight Crisis
This sneaky low can go unnoticed.
Risks: Confusion, seizures, or worse if untreated.
Fix: Bedtime snack with protein + carbs if levels are borderline. Continuous glucose monitors (CGMs) provide alerts.
Sleep Apnea: The Double Threat to Diabetes
Breathing pauses disrupt oxygen, worsening insulin resistance.
Story: Mark, 64, a truck driver from Ohio, snored loudly and felt exhausted. CPAP therapy + weight loss improved his A1C dramatically.
Tips: Side sleeping, weight management, avoid alcohol.
Nighttime Thirst and Frequent Urination (Nocturia)
Waking thirsty or to pee multiple times?
Cause: High blood sugar pulls fluid into urine.
Action: Monitor levels. Limit fluids after 7 PM. Control daytime intake.
Self-check: How many bathroom trips nightly? Above 2 is concerning.
You’re in the top 40% of committed readers—keep going!
Nighttime Leg Cramps: A Painful Warning
Sudden, intense cramps disrupt sleep.
Why: Electrolyte imbalance or poor circulation from high glucose.
Relief: Hydrate, stretch calves pre-bed, ensure magnesium/potassium.
The Ultimate Sign: Nocturia as the #1 Red Flag
Frequent nighttime urination tops the list.
Why it’s dangerous: Signals persistently high blood sugar, risking complications.
Real transformation: Linda, 62, from California, woke 4–5 times nightly. Better daytime control reduced trips to once. “My energy skyrocketed,” she said.
Your 8-Week Sleep-Improving Action Plan
| Week | Focus Sign | Daily Action | Expected Benefit |
|---|---|---|---|
| 1–2 | Night Sweats + Hypoglycemia | Bedtime check + carb snack | Fewer interruptions |
| 3–4 | Restless Legs + Cramps | Evening stretches + hydration | Calmer legs |
| 5–6 | Sleep Apnea + Thirst | Side sleeping + fluid timing | Deeper rest |
| 7–8 | Nocturia + Overall | Consistent glucose monitoring | Restored energy |
Comparison: Signs vs. Quick Fixes
| Sign | Common Misdiagnosis | Better Approach | Potential Outcome |
|---|---|---|---|
| Night Sweats | Menopause/Hormones | Glucose check | Stable levels |
| Restless Legs | Stress | Neuropathy management | Less tingling |
| Nocturnal Hypoglycemia | Bad dreams | Bedside carbs | Safety net |
| Sleep Apnea | Snoring | CPAP/weight loss | Better oxygen |
| Nighttime Thirst | Dehydration | Sugar control | Fewer trips |
The Ultimate Revelation: Blood Sugar Control Is the Master Key
The one thing tying everything together? Consistent blood sugar management—through diet, meds, monitoring, and lifestyle—turns these nighttime dangers into manageable blips.
Imagine 30 days from now: Sleeping deeply, waking refreshed, feeling energized all day. The cost of ignoring these signs? Worsening diabetes, fatigue, complications. The reward? Better health, sharper mind, more joy.
Start today: Check your blood sugar tonight.
You’re now in the elite 5% club—congrats!
This article is for informational purposes only and does not replace professional medical advice. Consult your healthcare provider for personalized guidance, especially if you have diabetes or suspect symptoms.
P.S. Ultimate insider tip: Keep a bedside “low kit” (glucose tabs + water)—only dedicated readers know this simple lifesaver!




