Imagine this: You’re going about your daily routine when something feels just a little off—a spot of unexpected bleeding after a routine moment, or a nagging ache you can’t quite place.
It’s easy to brush it aside as “nothing serious,” but what if that whisper from your body was trying to tell you something important? Stories like Sarah’s, a vibrant grandmother in her 50s, remind us why paying attention matters.
She ignored a subtle change for months, only to learn it was an early hint of cervical cancer that, caught sooner, might have been even easier to address. Could tuning into these quiet signals make all the difference for you?
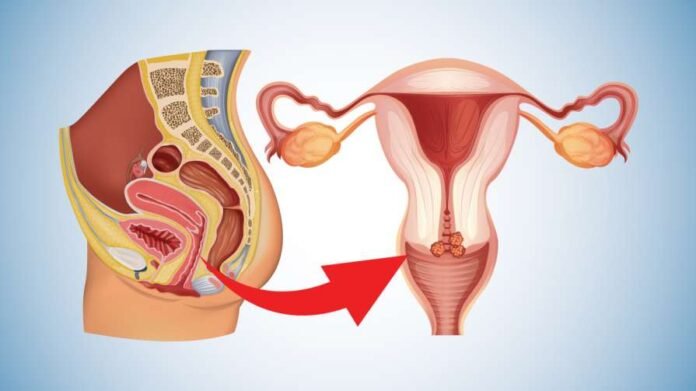
You might think you’re too busy or too healthy to worry, but cervical cancer sneaks up quietly. The cervix, that narrow passage connecting your vagina to your uterus, is where this cancer often begins, usually from changes in cells over time.
Early on, it rarely announces itself with fanfare—many women, especially those over 30, go years without a clue.
For folks like you, juggling family, work, or grandkids, it’s tempting to chalk up odd symptoms to stress, hormones, or just getting older.
But ignoring them can let potential issues grow, turning a manageable situation into something more challenging.
The real urgency hits when you realize how common this is. Every year, thousands of women face this diagnosis, and while screening has cut rates dramatically, gaps remain—especially if you’ve skipped a check-up or two.
Women in their 30s to 50s are often at higher risk, particularly if you’ve had multiple partners, started intimacy young, or smoke—factors that can invite the human papillomavirus (HPV), a common virus linked to most cases.
Without early attention, what starts as cell changes can spread, affecting your energy, comfort, and peace of mind.
Think of it like a slow leak in your roof: a small drip today becomes a flood tomorrow if you don’t peek up there.
And the consequences? Fatigue that steals your joy in simple things, like playing with the kids or gardening on a sunny afternoon.
Unexplained pain that disrupts sleep or daily tasks. For older adults, this can compound other age-related tweaks, making mobility or intimacy feel burdensome.
But here’s the heart of it: when spotted early, outcomes can be so much brighter, often with simpler steps to get you back to feeling like yourself. Who wouldn’t want that extra layer of reassurance?
Now, let’s build a little suspense—because knowledge is power, but only if you stick around to claim it. We’re going to count down five key signs that research from trusted health experts highlights as potential red flags you shouldn’t dismiss.
We’ll tease them out one by one, with real-talk stories to make them stick, and save the one that sneaks up on so many for last. Trust me, by the end, you’ll feel equipped, not scared.
First mini-reward: Understanding even one sign could spark that “aha” moment you’ve been waiting for.
Starting with number five: unusual vaginal discharge. You know your body best—if things suddenly shift to something watery, bloody, or with a foul odor that wasn’t there before, it might be worth a chat with your doctor.
Some studies suggest this can signal cell changes in the cervix, though it’s often tied to simpler issues like infections. Take Lisa, a teacher in her 40s, who noticed a change during a busy school year.
She thought it was just stress, but a quick check revealed precancerous cells—caught early, treated simply, and now she’s back to grading papers without a worry. See? That mini-hook of awareness can lead to real peace.
Dropping to number four: heavier or longer periods than your norm. If your monthly flow feels like it’s overstaying its welcome or packing more punch, it could be an under-recognized nudge from your body.
Research indicates this might happen as abnormal cells irritate the cervical lining, but again, it can stem from hormonal shifts or fibroids too.
Picture Maria, a retiree enjoying her golden years, who waved off her extended cycles as “part of the change.”
A routine visit turned the tide—early intervention meant no big disruptions. You’re already halfway through our countdown, feeling that curiosity build?
Number three: pain during intimacy or a dull pelvic ache. That uncomfortable twinge after being close with your partner, or a vague pressure in your lower belly, isn’t something to tough out silently.
It may point to inflammation or growths pressing on nearby tissues, per health guidelines, though everyday strains like muscle tension are common culprits.
Remember Aunt Ellen from the family reunion? She shared how ignoring that subtle discomfort led to a diagnosis, but early action kept her dancing at weddings.
Here’s your next mini-reward: Realizing these aren’t just “women’s woes” but signals worth honoring.
At number two: bleeding between periods or after menopause. Spotting when you least expect it—mid-cycle, post-hug with your spouse, or years after your periods bid farewell—can feel alarming.
Experts note this as a frequent early whisper, possibly from fragile blood vessels in changing cells, yet it might also flag polyps or hormone dips. Like countless others, you deserve to know it’s okay to ask.
And now, the drumroll for number one—the sign that flies under the radar for so many, yet packs the biggest payoff when addressed promptly.
Drumroll please: unexplained lower back or leg pain, often with swelling. That nagging ache in your back or a heavy feeling in your legs might seem like sciatica or long days on your feet, but if persistent, it could hint at the cancer nudging nearby nerves or lymph nodes. Studies suggest this emerges as things progress, but catching it here means options abound for relief.
Meet Joan, 62, who mistook her leg fatigue for arthritis—turns out, it was an early alert. A prompt screening and treatment got her hiking again. There it is: the game-changer reveal that turns “what if” into “I’ve got this.”
So, what’s the empowering next step? Knowledge without action is just trivia, right? The solution starts with tuning in—keep a gentle journal of any changes, no judgment, just notes. But the gold standard? Schedule that Pap test or HPV screen if it’s been a while.
These simple swabs can spot cell shifts years before symptoms shout, giving you a head start that research shows can make all the difference.
You can chat with your doctor about your history—maybe add the HPV vaccine if eligible, or quit-smoking support if that’s your hurdle. Remember, these are tools that may help safeguard your wellness, not guarantees.
Always consult a healthcare professional for advice tailored to you, as what works for one might need tweaking for your unique story.
Let’s make it practical: Block 15 minutes this week to call your clinic and book that check-up. Or, if something from our list rings a bell, jot it down and share it at your next visit.
Pair it with self-care, like a short walk to clear your head or a chat with a trusted friend about screenings—they might need the nudge too. You’re not alone in this; health pros are there to guide you gently.
You’ve made it this far— that’s a win already. These signs aren’t meant to worry you but to whisper, “Hey, let’s check in.”
By staying curious and proactive, you’re gifting yourself more mornings with coffee on the porch, more laughs with loved ones.
This week, take that small step: Reach out to your doctor about a screening or any nagging feeling. Then, drop us a note here—how did it go? Sharing your story might just light the way for someone else.
This article is informational only and does not replace professional medical advice — recommend readers consult a qualified healthcare provider for personalized guidance.